The objective of this page is to provide you sample cases to practice insulin adjustment. This page is in development and will grow. For access to formal online learning modules for healthcare providers with automatically marked quizzes, please click here.
MEDICATIONS
ARTHUR: What do you suggest for an insulin dose tonight? Current dose is 7 units basal.
- 38 years old, DM x 5 years, 68 kg, lean and active (may be LADA)
- Started glargine (Basaglar) a few days ago as fasting readings were 10-11 mmol/L.
- Currently 7 units basal insulin at night.
- Metformin 1000 mg b.i.d.
- Secretagogue: Gliclazide (Diamicron®) 160 mg b.i.d.
- DPP-4i: Sitagliptin (Januvia®) 100 mg daily
- A1c 7.6%
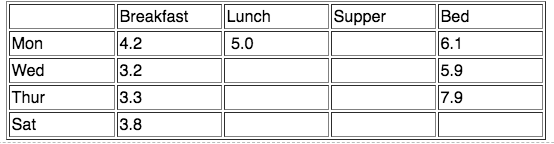
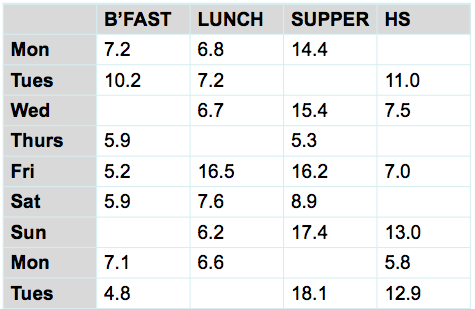
- Current glucose readings, since starting insulin, are below.
| Breakfast | Lunch | Supper | Bed | |
| Tues | 9.9 | 7.1 | 8.1 | |
| Wed | 10.7 | 6.8 | ||
| Thur | 10.3 | 7.9 | ||
| Frid | 11.2 |
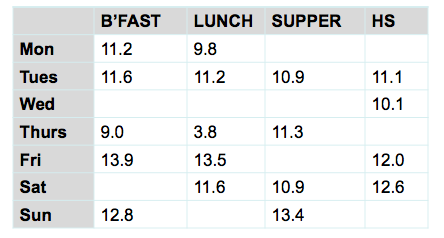
Type 1 x 18 yrs, A1c 6.2%, 70 kg. More active at work recently and no plans for this to stop. He doesn’t want to eat more as a permanent solution. He senses his lows and has never had a severe low. Degludec (Tresiba) 39 units qam; ICR 1:10; ISF=2; TDD = 62 units
1. What is the main glucose problem or pattern?
- A. Low pattern at 1 time of day
- B. Low pattern every 1 day of the week (e.g. every Wed)
- C. Significant lows at varied times of the day
- D. Highs – a pattern of highs, or mostly high everywhere
- E. Erratic at each time of day (1/2 in target at each meal & 1/2 over target at each meal)
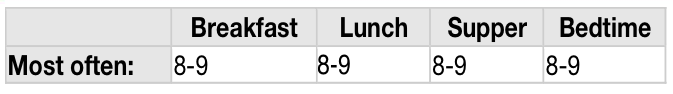
2. These are some suggestions from the Insulin Adjustment page for the pattern he's experiencing. What do you suggest? Remember: Tresiba 39 units/day. TDD = 62 units. Senses lows. No severe hypo. More active at work with no plans for this to stop. Pick 1 answer. (poll workshop)
- A. If events are explainable (exercise, vacuuming, over-bolused, under-ate, alcohol, weight loss), ask patient about methods to prevent lows. It may or may not include insulin adjustment.
- B. If a pattern at one time of day exists, reduce insulin most responsible (eg. lows at supper, reduce lunch bolus)
- C. If significant low readings at varied times of the day (low everywhere), either decrease basal dose if > 60% TDD or decrease bolus insulins if basal is < 40% TDD.
- D. If lows follow high readings assess ISF and check that client is not stacking corrections
Resource: Adjusting for hypoglycemia on Insulin Adjustments page
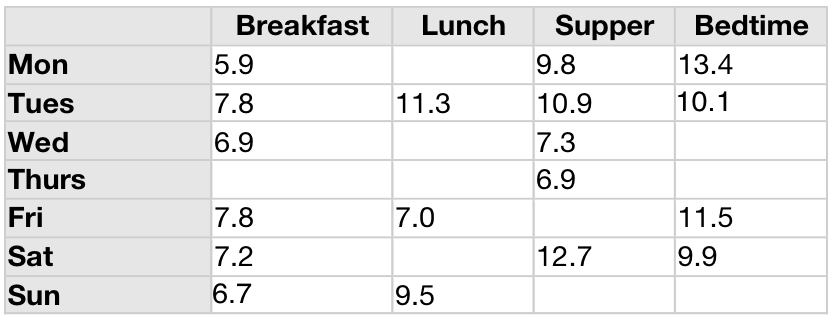
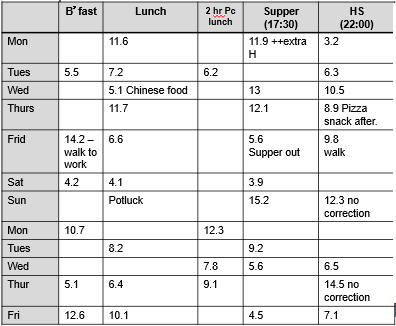
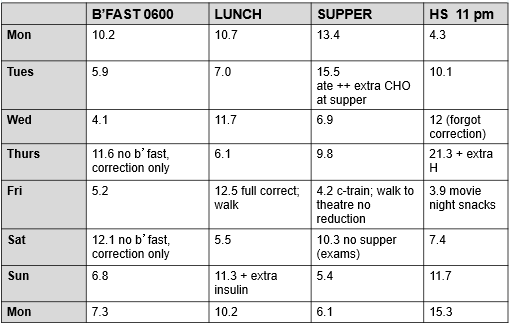
Sullivan has type 1 diabetes and is targeting A1c < 7.0%. When over target, he gives correction insulin unless he's made a comment otherwise. You clarified that all of the readings below are before meals e.g. at least 3 hours since food.
Remember the steps: (After assessing for safety and verifying this is erratic and no patterns.)
1: Assess overnight basal
2: Assess meal boluses
3: Assess ISF
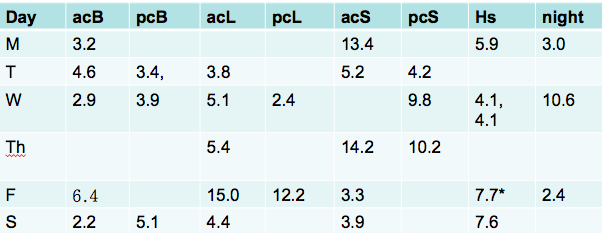
 |
|
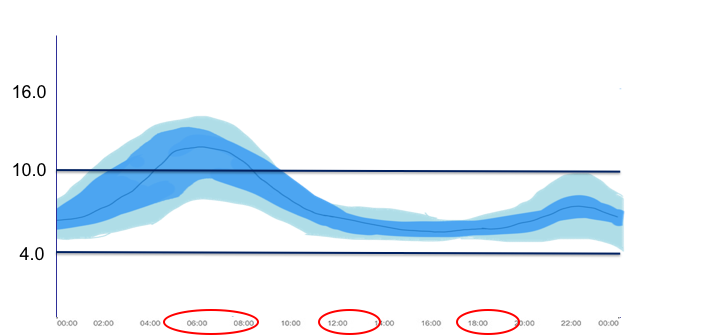
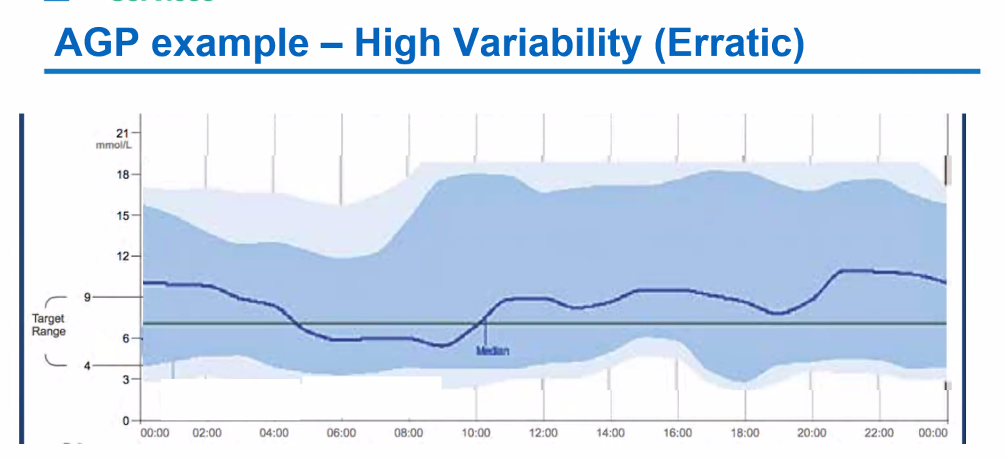
If it was a sensor, the AGP would like similar to below.
What do you suggest to address the problem? Pick one.
- A. Increase basal insulin (degludec)
- B. Change ICR to give more bolus
- C. Change ICR to give less bolus
- D. Change ISF
Resources: