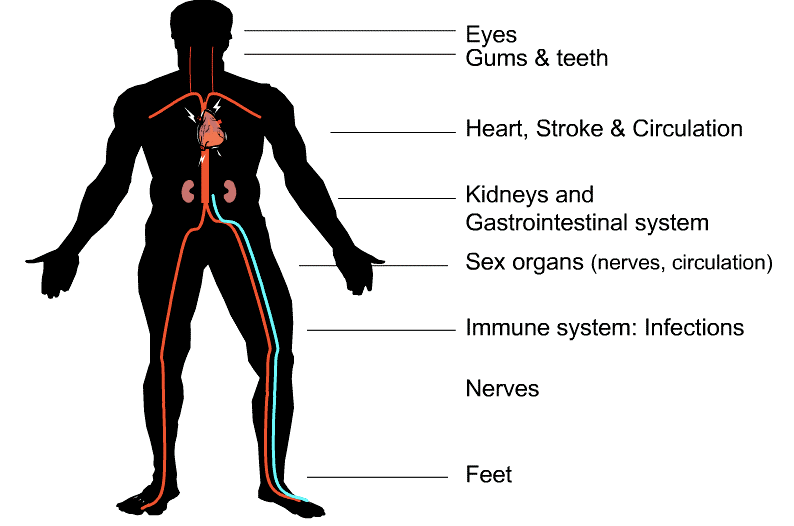
This section provides a brief overview of common diabetes complications along with how to screen, prevent and manage them.
Possible problems:
- Retinopathy
- Glaucoma
- Macular Edema
- Cataracts
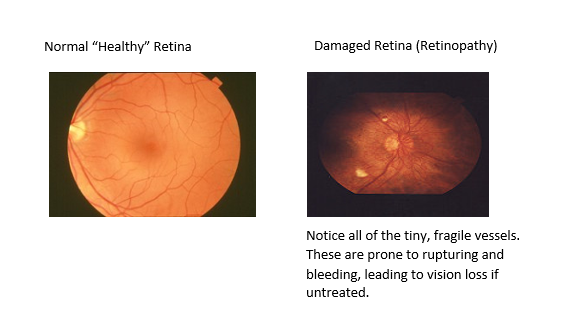
Ideas for teaching about retinopathy:
Retinopathy is damage to the blood vessels at the back of the eye. Only a doctor can see this damage with a special eye exam where pupils are dilated. There are usually no early warning signs that damage is happening.
Picture courtesy of National Eye Institute: https://nei.nih.gov/
How to test?
Eye exam (dilated retinal exam) every 1-2 years.
How to prevent, treat and manage?
- Target A1c
- Blood pressure less than 130/80
- Possible need for laser, medicine or surgery
More information: Retinopathy page
Possible problems:
- Heart attack (Myocardial Infarction)
- Stroke
- Peripheral Arterial Disease (PAD)
Ideas for teaching:
High blood sugars can damage the smooth inner lining of blood vessels, much like using a metal spatula on a teflon (non-stick) frying pan. What happens to your egg when you use the damaged frying pan? It sticks!

Picture courtesy of Pixabay
Similarly, as blood fats move through the vessels, they can stick more to the insides of the vessels, leading to blockages. A blockage in the heart could result in a heart attack; in the brain it could cause a stroke, and in the outer limb vessels this can lead to peripheral arterial disease.
Some educators also like to use 'glucose wands' to visually demonstrate circulation slowed down by blood high in sugar.
How to test:
- Blood pressure check at least once a year and more often if elevated
- Lipids (cholesterol levels) checked every 1-3 years, or more often if indicated
How to prevent, treat and manage:
- Target A1c
- Blood pressure less than 130/80
- ACE inhibitor or ARB
- Statin medication
- ASA for secondary prevention
- Some diabetes medications
- Lifestyle: smoking cessation, healthy nutrition, exercise, stress reduction
More info: Vascular Risk Reduction
Possible problems:
Kidney disease (nephropathy)
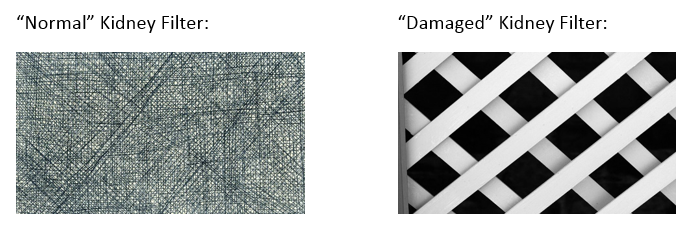
Ideas for teaching:
High blood sugars can damage the filters in our kidneys so that they can no longer filter our blood properly. This causes beneficial proteins to leak into the urine and waste products to build up in the blood.
You can compare damaged kidney filters to a coffee filter that has 'holes' poked in it. The coffee filter can no longer do its job keeping the grounds in, and the water passing through.
How to test:
- Annual urine test (random): Albumin to Creatinine Ratio (ACR)
- Annual serum creatinine to measure eGFR
How to prevent, treat and manage:
- Target A1c
- Blood pressure less than 130/80
- ACE inhibitor or ARB
- Some diabetes medications may help protect the kidneys
- Other medicine for chronic kidney disease, possible dialysis
More info: Nephropathy page
Possible problems:
- Peripheral neuropathy - pain or loss of sensation to hands/legs/feet
- Autonomic neuropathy (gastroparesis, bowel/bladder problems, blood pressure regulation, hypo unawareness, changes to perspiration)
- Foot concerns leading to amputation
- Sexual problems such as erectile dysfunction
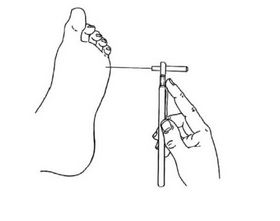
Ideas for teaching about peripheral neuropathy:
High blood sugars, along with poor circulation can be very irritating and damage fine nerve endings so that sense of feel or touch is lost. We often see this first in the feet - being the furthest away from the heart and brain. This is why a yearly foot check by a health care professional is so important to detect beginning signs of nerve damage.
Picture courtesy of guidelines.diabetes.ca (2018 Diabetes Canada)
How to test:
- Annual foot exam, or more often if any concerns
- Screening questions for any gastrointestinal or sexual function problems
- Possible nerve conduction, gastric emptying tests
How to prevent, treat and manage:
- Check feet daily and follow good foot hygiene
- Target A1c
- Various strategies to help manage gastrointestinal problems and diabetes management challenges
More info: Neuropathy page and Foot Care
Possible problems:
- Dental problems such as gingivitis and periodontitis
- Foot wounds leading to amputation
- Urinary tract infections
- Influenza or other viral infections
Ideas for teaching :
Infections may be more problematic when blood sugars are high as (just like most of us) bacteria loves sugar!
How to test:
Patients are encouraged to seek medical attention whenever they have signs or symptoms of an infection as soon as possible.
How to prevent, treat and manage:
- Annual dental exam
- Vaccines: routine vaccinations as recommended for general population plus pneumococcal vaccination.
- Good foot hygiene and daily foot checks
- Good hand hygiene (properly washing hands)
More info: Foot Care

Meet Betty, a 45 year old woman who has had type 1 diabetes for 30 years. She tells you that she has been struggling to control her blood sugars, often dropping low 1-2 hours after eating. She has been losing weight due to poor appetite and feels nauseated when she is able to eat. She tells you she often feels like food is sitting 'like a lump' in her stomach.
What diabetes complication may Betty be experiencing and need further investigation for?
What strategies can we suggest to help Betty manage her blood sugars with this complication?
Click here for discussion answers
Case #2:
Ken has had type 2 diabetes for 30 years and is being followed by nephrology for CKD- Chronic Kidney Disease. His GFR is 15. A1c 7.5%.
Current diabetes medications include Gliclazide (secretagogue) 160 mg twice a day and Sitagliptin (DPP-4 inhibitor) 25 mg once a day.
Upon assessing safety factors you find out that Ken is waking in the morning with low blood sugars. He will also have about 4-5 low blood sugars per week during the day.
What could be the reason(s) for Ken's low blood sugars?
What kind of treatment strategies might you suggest?