The objectives of this page are to:
- Provide guidelines for insulin adjustment
- Provide related resources, including adjustment cases for practice
Note: In September 2022, AHS released the Diabetes Medication Adjustment Protocol (Adults) intended for use by health care professionals (with diabetes management expertise) who work in a specialty diabetes out-patient centre in the adjustment of antihyperglycemic medications.
Topics
- Variables Impacting Dosing Suggestions
- Basic Insulin Adjustment Table
- Basal Insulin Adjustments
- Bolus Insulin Adjustments
- **Adjustments for Patterns in BBIT**
First, identify the glucose pattern. Then choose from the options under these headings:
- Hypoglycemia (pattern or low everywhere)
- Hyperglycemia (pattern or high everywhere)
- Erratic Pattern
Related:
Variables
Consider the following prior to adjustment of insulin, as solutions might exist here. You may also wish to view the Hypo & Hyper Troubleshooting Chart .
|
|
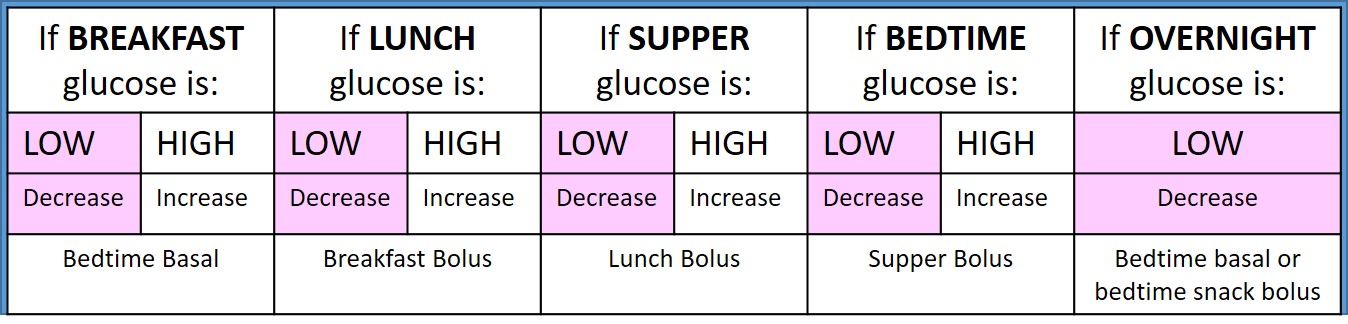
Basic Insulin Adjustment Table
Notes:
- The chart above is simplified. There are many factors to consider, including the "basal bolus split". The sections below will address more details, step-by-step.
- Remember, patterns of lows or frequent lows are usually addressed first for safety! Depending on the patient and their frailty level, 1-3 episodes of hypoglycemia a week may be acceptable if self-managed and present with symptoms.
- In BBIT, the role of basal insulin is usually different compared to those taking just basal insulin. In BBIT, the role of basal is usually to hold glucose readings stable overnight to within a few mmol/L ideally. E.g if readings are 10 mmol/L at breakfast, in target mostly at lunch & supper, but 10 mmol/L at HS (bedtime), the basal dose in BBIT is likely doing great! It is holding readings stable from bedtime overnight till morning, helping the body utilize the glucose made by the liver. (The problem though is starting with high HS readings. It's key to ask, "Where is the problem starting?" Then try to prevent it.)
- High fasting readings in BBIT may require increasing basal if in target at HS or may require addressing either high bedtime readings first or the bolus given with bedtime snack. Again, It's key to ask, "Where is the problem starting?"
- If almost all readings are high, see options below for high everywhere. If numerous lows over the day, see options below in hypoglycemia.
- The above table is adapted from Alberta Health Services' Basal Bolus Insulin Therapy www.bbit.ca
Basal Insulin Adjustment
1. FOR BASAL INSULIN ONLY (no bolus insulin prescribed)
- Historically, the goal of "basal only" insulin was to drop fasting readings into target. Then, agents-other-than-insulin would ideally work to keep the glucose readings in target during the day. Now-a-days, basal insulins may not have peaks to target fasting readings, but still, fasting readings are often the easiest to use to assess basal doses.
- (Of note in BBIT, basal insulin is ideally titrated to hold glucose readings stable, particularly overnight. e.g. to address glucose produced by the liver, not glucose derived from food.)
- Adding basal insulin to oral/injectable agents in type 2 diabetes is a gentle way to add in insulin to bring glucose readings into target with less weight gain and hypoglycemia than starting with bolus/meal insulin first.
- Please note, AHS Diabetes Medication Adjustment Protocol (Adults) requires adjustments exceeding 20% of the current total daily dose to require review, direction and an order from the patient’s Physician, Nurse Practitioner or designate). Exception: Orders are not required if the specialty diabetes out-patient centre's resource documents so indicate.
- Basal Only - Insulin Adjustment Notes (there is no one "right" way):
- Please remember: Insulin adjustment is not just about choosing a dose; it is an important collaboration between clinician and patient. Please consider asking e.g. "How do you feel about increasing that dose?" Assessing conviction & confidence can be reviewed here.
- 1 unit per day till in target.
Exceptions: Degludec (Tresiba) is titrated by 2 units every 3-4 days or 4 units once a week (Diabetes Canada) and icodec (Awiqli) is adjusted weekly e.g. 10% to the nearest 10 unit increment. - 2 units or 10% every 1-2 days is common advice.
As doses increase, focus on the percent adjustment. A 2 unit increase on 40 units is only a 5% adjustment. It may be more appropriate to suggest a 4 unit (10%) increase every few days. - 10-20% or greater is a frequent guideline for clinicians. Keep in mind your organization's adjustment protocols.
Consider glycemic responses to past adjustments. If newer to basal, consider comparing dose to the conservative BBIT based formula for starting basal insulin. e.g. 100.0 kg patient started on 8 units basal insulin, but no drop in glucose readings afterwards. Consider more than 10% increase given that the formula suggests a starting dose of 10-20 units. - For adjusting ultra-long acting basal insulins like degludec (Tresiba - once daily dosing, 42 hr duration) and icodec (Awiqli - once weekly dosing) see product comments in the Complete Medication Table.
- Consider adding bolus insulin once basal dose starts exceeding 0.5 units/kg (e.g. if 90.0 kg and taking more than 45 units basal insulin). Refer to Insulin Formulas. This is a general guideline and is individualized by prescribers, as some patients can be very insulin resistant and may benefit from more concentrated basal insulin.
- For sample basal adjustment cases, visit here.
- Please remember: Insulin adjustment is not just about choosing a dose; it is an important collaboration between clinician and patient. Please consider asking e.g. "How do you feel about increasing that dose?" Assessing conviction & confidence can be reviewed here.
2. FOR BASAL + BOLUS INSULIN
- Adjust basal dose to hold glucose readings stable (within approx 2 mmol/L) from bedtime to morning, assuming no evening snack is eaten.
- If an evening snack is eaten, remember that overnight and morning readings may also be impacted by that evening bolus (or lack of bolus).
Bolus Insulin Adjustment
Use the Basic Insulin Adjustment Table to determine which meal's bolus insulin needs adjusting.
- ADJUSTING "SET" or "FIXED" or "BASE" MEAL BOLUSES
These are all names for meal boluses that stay the same each day for the same meal e.g. lunch is always 10 units. A correction is added if needed. These "set, fixed or base" meal boluses (however your patient or you refer to it) are usually appropriate for those who eat fairly consistent meals from day to day. Here are 3 ways to adjust these boluses.
- A. Adjust the dose by 10% - 20% or as deemed appropriate. Consider how the last adjustment worked. If the patient is newer to bolus insulin, consider referencing the BBIT formula for starting bolus insulin to be sure the dose is minimally adequate.
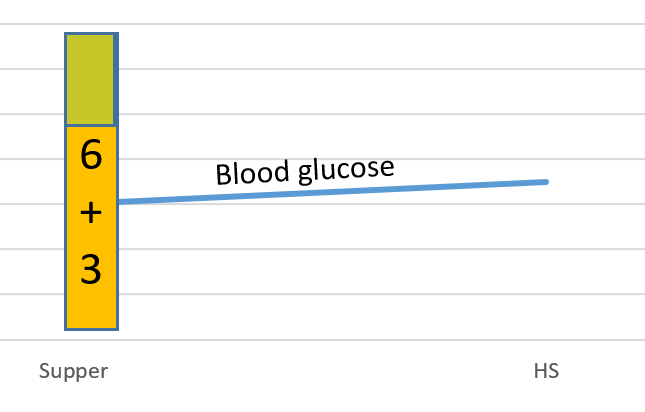
e.g. A suggested starting bolus dose for 120.0 kg patient is 6 - 12 units per meal using BBIT. If the patient arrives on 4 units per meal (per Diabetes Canada start dosing), you might feel more comfortable making bigger increases. - B. Add the correction dose from the meal that follows, if a dose increase is needed at a meal. (Or reworded, if high readings at a mealtime, such as suppper, take the units of correction dose at supper and add to the previous meal's bolus dose - which is lunch in this case - to prevent the high.)
e.g. Mrs. Wurther gives set meal boluses and a correction if over 7 mmol/L. Here are her current readings and meal doses.
B'FAST LUNCH SUPPER
5 units 5 units 9 units + 3 units correction (ISF 2)
5-7 mmol/L 5-7 mmol/L 13 mmol/L
The new meal bolus dose at lunch would be 5 units + 3 units = 8 units
e.g. 3 units added to lunch to prevent high readings at supper
Going forward, at lunch she would give 8 units + correction if needed. Hopefully going forward, she won't need so much correction at supper. - C. Find meals where total meal + correction dose holds readings stable to the next meal. This becomes the new "set" or "base" meal dose.e.g.
12 mmol/L at lunch.
Gave 10 meal bolus + 3 units correction.
12 mmol/L at supper.
The full 13 units covered the food and kept glucose readings level, but did not correct the high reading. Therefore, 13 units is new meal base dose + correction if over target.
- A. Adjust the dose by 10% - 20% or as deemed appropriate. Consider how the last adjustment worked. If the patient is newer to bolus insulin, consider referencing the BBIT formula for starting bolus insulin to be sure the dose is minimally adequate.
- ADJUSTING CARB RATIOS [sometimes termed INSULIN TO CARBOHYDRATE RATIOS (ICR)]. Choose 1 option.
- A. Change the carb value, for example
- If LOW afterwards, increase the carb value
Carb Ratio = 8, consider new Carb Ratio = 9 or 10
Carb Ratio = 10 consider new Carb Ratio = 12
Carb Ratio = 12 consider new Carb Ratio = 15
Carb Ratio = 15 consider new Carb Ratio = 20 - If HIGH afterwards, reduce the carb value.
Carb Ratio = 20 consider new Carb Ratio = 15
Carb Ratio = 15, consider new Carb Ratio = 12
Carb Ratio = 12, consider new Carb Ratio = 10
Carb Ratio = 10 consider new Carb Ratio = 9 or 8
Carb Ratio = 9, consider new Carb Ratio = 8 - B. Add typical correction dose to previous meal
- If HIGH afterwards, consider adding the correction dose from the following meal. (Or reworded, if highs at a mealtime, take the units of correction dose and add to the previous meal's bolus dose.)
e.g. Mr. Toystore, Target: 7 mmol/L
Carb Ratio of 10 for all meals
ISF 2
Supper: 4-7 mmol/L, 60 g carb common, 6 units meal bolus
Bedtime: 13 mmol/L (no snack) + 3 units correction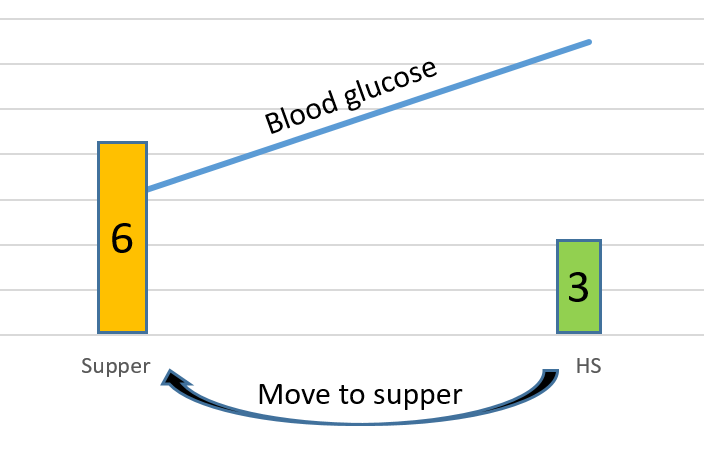
The new supper Carb Ratio = 60 g carb divided by 9 units (i.e. 6+3)= approx 7
Going forward, his Carb Ratio is 10 at breakfast; 10 at lunch; 7 at supper - C. IF high or low at all meals, consider 500/tdd
- If you've determined that the Carb Ratio at all meals needs to change based on the basal/bolus split, consider using the 500 rule as a reference (500/TDD= Carb Ratio).
e.g. Bob's current Carb Ratio is 10.
TDD = 60 units.
500/60= approx 8
HIs new Carb Ratio for all meals is 8.
(The use of this formula may not apply to each individual, but may help to suggest a direction for Carb Ratio adjustment.)
- ADJUSTING INSULIN SENSITIVITY FACTOR (ISF or Correction Factor)
- Remember:
- Standard formula is 100/TDD = ISF
- ISF of 1 means: 1 unit of bolus insulin drops glucose by 1 mmol/L.
- ISF of 2 means: 1 unit of bolus insulin drops glucose by 2 mmol/L.
- ISF of 3 means: 1 unit of bolus insulin drops glucose by 3 mmol/L.
- Assess ISF by:
- Comparing current ISF to formula for ISF (100/TDD) and/or
- Finding times where only correction insulin was used (no meal and no meal bolus) and/or
- Assessing if lows often follow high readings and/or
- Finding ac meal times above target and assessing subsequent readings (only if you've verified the meal bolus works when ac readings in target) and/or
- Considering some frequent observations: Those who are lean and/or very active or sensitive to insulin often have an ISF of 3 or 4, occasionally more. (One unit drops them "a lot".) Those with overweight or insulin resistance or less active, may have an ISF of 1.5 or 1 or occasionally less. (One unit drops them "a little".) On occasion, these observations do not apply. An individual's insulin & glucose data is the most reliable source.
- See examples of above on ISF page
- Also assess that patient is not "stacking" corrections e.g. giving too many too soon.
- Adjust ISF:
- If giving hypoglycemic results, increase the number e.g. ISF 2 becomes ISF 3
- If giving above-target results, decrease the number e.g. ISF 3 becomes ISF 2
- For Adjusting a Correction Scale see our ISF page.
- Remember:
Adjusting for Patterns in BBIT
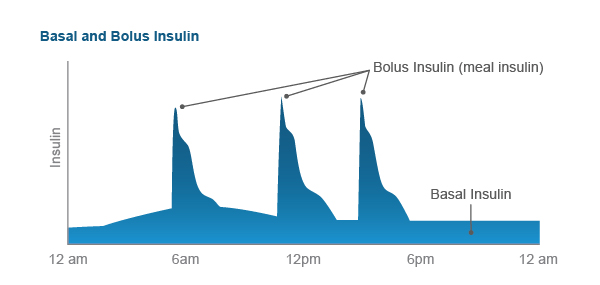
Basal Bolus Insulin Therapy (BBIT) attempts to mimic physiologic insulin needs by providing insulin for food (bolus) and insulin to cover the glucose made by the liver overnight and between meals (basal). Which insulins need adjusting depend on the glucose data or "pattern". As well, adjustments to address patterns may take into account the basal/bolus split. Often, basal needs are 40-60% of Total Daily Dose (TDD) insulin. You'll read more on this in the strategies to address hypo or hyperglycemia below.
Strategies for addressing each pattern are reviewed below.
- Hypoglycemia - frequent patterns or low everywhere
- Hyperglycemia - frequent patterns or high everywhere
- Erratic pattern
Notes:
- Quite often, we'll refer to the percent basal or the basal/bolus split. Physiologically, 40-60% of total daily insulin is usually basal. It's useful to know this split when making some adjustments. (There are exceptions of course. Notably, those on low carb diets will have a high % basal since they aren't taking much bolus insulin.)
- Basal insulin is at an appropriate dose when it holds glucose readings stable within a few mmol/L from night till morning, assuming no food. (most of the time)
- Severe episodes of hypo and hyperglycemia (DKA, HHNK) are not addressed here. They are reviewed in the Safety Checklist.
- Review sample BBIT Adjustment Cases.
Adjusting for Hypoglycemia
Reminders about lows (also in the Safety Checklist):
- Not all episodes of "lows" will be in logbooks. Patients often don't indicate events as "lows". They may have their own definition. Clarify by asking, "How often are your readings below 4 mmol/L? How often are you are weak, shaky, sweaty?"
- Troubleshoot prevention of frequent lows as the priority, even if there is a pattern of hyperglycemia. Remember almost everyone on BBIT will have occasional "lows" which should not, in most cases, prevent you from adjusting insulin to fix patterns of "highs".
- Remember to assess how patients treat lows and the symptoms they have. These can change over time.
- If there is hypoglycemia unawareness or recurrent severe lows requiring the help of a third party, set a higher glucose target (educate using patient handout) and find an option below to resolve the problem.
IF THREE OR MORE LOWS PER WEEK
(less if elderly, frail, or severe low or hypo unawareness)
Options:
- If events are explainable (exercise, vacuuming etc, over-bolused, under-ate, alcohol, weight loss etc), ask patient about methods for preventing these lows. It may include insulin adjustment, it may not.
- If a pattern exists, reduce insulin most responsible per the basic insulin adjustment table (eg. lows before supper, reduce lunch bolus)
- If significant low readings over the entire day (low everywhere),
- Consider basal insulin decrease (especially if basal insulin is > 60% of total daily dose of insulin (TDD). However, those on low CHO diet usually have an appropriately higher % basal.)
- Consider bolus insulin decrease (especially if bolus insulin is > 60% of TDD)
- If lows follow high readings
- Assess ISF to see if appropriateAssess ISF to see if appropriate
- Check that client is not stacking corrections (giving too many, too soon)
- If no pattern consider asking client to record meal, activity, dose etc. that come before each low to help problem-solve.
- If on a sliding scale, look to see if the lows are related to using one or two rows of the sliding scale. E.g. 11.1 -13 mmol/L range of the supper scale. See adjusting correction scales on ISF page.
Adjusting for Hyperglycemia
OBVIOUS HIGH PATTERN e.g. mostly high at lunch. Options:
- Review insulin(s) affecting that time of day. Determine the best one to adjust.
 e.g. if supper readings high:
e.g. if supper readings high:
- increase lunch bolus OR
- if in target at pm snack but elevated before supper then add/increase snack bolus OR
- if in target after lunch, no snack, but elevated by supper then investigate increased afternoon basal insulin or a basal with longer duration
. - If adjusting a sliding scale, carefully consider if all of the glucose ranges on the scale ( e.g. 4-7, 7.1-9, 9.1-11, etc) need an adjustment, or if just a few of the ranges require an adjustment. See adjusting correction scales on ISF page.
HIGH EVERYWHERE e.g. few in target. Options:
- Consider addition of agents other than insulin such as an SGLT, GLP-1, metformin
- Consider increasing basal dose, especially if basal is less than 40%-60% TDD
- Consider increasing bolus insulins if basal is > 60% TDD
- Pick the highest of the high readings to target first
- Address fasting glucose first (supper bolus might need a change to prevent HS elevations; HS snack bolus might need a change)
- Increase one of the meal boluses, ideally patient's choice, to break the pattern or until a pattern appears.
- If a prescriber in hospital, consider increasing TDD by 10-20% and recalculating all Basal, Bolus and Correction Doses. (This may be a confusing strategy for outpatients who would then be using all new basal and bolus doses or formulas).
Adjusting for Erratic Readings on Basal Bolus Insulin Therapy (BBIT)
In erratic glucose patterns, most meals (testing times of the day) have a fairly even mix of high and in-target readings. e.g. Erratic most times of the day (1/2 at target, 1/2 above target). The following are suggested steps to follow.
1: Assess overnight basal
2: Assess meal boluses
3: Assess ISF
ERRATIC STEP 1: Assess and adjust evening basal insulin to start the day in target.
Glucose readings that are stable (within approx 2 mmol/L) from evening to morning with no snack usually indicate appropriate overnight basal dosing. If not stable, adjust basal.
ERRATIC STEP 2: Determine if meal boluses are adequate for each meal.
- Find pre-meal readings that are in target for each meal. If the subsequent readings are mostly...
- in target (with no snack in-between) then the preceding meal bolus is reasonable. eg. B’fast 6.1 mmol →Lunch 7.1 mmol
- elevated (with no snack in-between), then increase the preceding meal bolus or subtract carb from breakfast ratio.eg. B’fast 6.1 mmol →Lunch 8.9 mmol. Increase b’fast meal bolus or adjust ICR (e.g. 1:10 goes to 1:8)
- low (with no snack and bolus), then decrease the preceding meal bolus or add carb to breakfast ratio. e.g. B’fast 6.1 mmol → Lunch 3.2 mmol. Decrease b’fast meal bolus or adjust the ICR (e.g.1:10 goes to 1:12)
- elevated with a snack in-between, and the glucose reading before the snack is in target, then either the snack needs decreasing or the snack requires a bolus e.g. Breakfast 6.1 mmol; before snack 7.8 mmol (in target as 2 hr pc) and ac lunch 13.3 mmol.
- If only a few glucose checks and those are above target, find a dose that most often keeps the glucose readings stable from one meal to the next e.g. Breakfast 11.4 mmol with 7 units rapid total (meal bolus + correction) with result of lunch 12.5 mmol/L. In this case, it appears 7 units is appropriate for the new meal bolus. The correction dose would still need to be added to this new meal bolus.