Topics
- Introduction to medication classes
-
- Use Diabetes Canada Interactive Tool
- Use Diabetes Canada Visual Flowcharts
(med choices, stepwise insulin addition, max doses & eGFR considerations)
- Drug Interactions
Related:
- AHS Diabetes Medication Adjustment (adults) protocol
- Patient Medication Handouts - includes "When you are sick"
- Complete Diabetes Medication Table
- Drug Product Database (Health Canada)
- Medication Adjustments for Low Carb Diets
- AB Blue Cross Coverage Database
- Nephropathy and Stage 5 CKD - Management of Diabetes for Individuals on Renal Replacement Therapies
- Renal Dosing Chart - Diabetes Canada
1. Introduction to diabetes medication classes
Drug classes differ by their mechanism of action, A1c lowering capacity, side effects, risk of hypoglycemia, effect on weight and vascular protection. Click the class headings below to review these and specific brand considerations. To view brand indications, doses and cost visit the Complete Diabetes Medication Table.
|
|
2. Questions to ask before medication changes
Prior to adjusting or adding more medications, consider these factors below:
- Glucose pattern or problem?
- Prior to adjusting or adding more medications, assess glucose patterns. Consider patterns of hypoglycemia first and then patterns of hyperglycemia. Basic pattern analsysis is here (click) and advanced pattern analysis (and insulin adjustments) are here (click).
- Patient's feelings about adding or increasing medications
- Keep client-centered approaches in mind. Consider asking, “How would you feel about increasing or adding another medication?” This can help assess conviction, barriers and permission.
- Variables impacting dosing suggestions:
Elements to consider prior to medication adjustment include the items below, as well as additional items in the small table of variables (link) and the big table of troubleshooting hypo and hyper (link). e.g. insulin integrity, lipohypertrophy, missed dosesetc.
- Keep client-centered approaches in mind: Glycemic control is frequently compromised by clients missing medication doses. To learn about the frequency of this in a nonthreatening manner, you may choose to use a normalizing statement such as, “Most people sometimes miss taking their diabetes pills. Life is busy after all. How often does this happen to you?”
- Level of Glycemia:
- How much does A1c or current glucose levels need to change to reach individualized target? Or does it, e.g. frail with A1c 8.0%?
- Will some drugs be more effective than others in getting A1c into target?
- Safety or Benefits - Will new medication or dose impact:
- Risk or reduction of hypoglycemia (commercial driver, frail elderly etc),
- Complexity or simplification of the new regime (move to combo meds: med+med or insulin+med)
- Comborbidities (benefits for CKD, HF, CVD, obesity or does dose need adjusting for CKD?)
- Risk of DKA (ability and willingness to test for ketones if increasing SGLT-2)
- Adherence:
- Will increased adherence impact glycemic control?
- Can a simplified regimen with combination medications or once daily versions of medications improve adherence? If yes, are they affordable?
- Lifestyle:
- Can lifestyle changes help to improve glycemia (e.g. what is duration of diabetes)? If adequate beta cell function remains in type 2 diabetes, lifestyle changes could potentially reduce A1c by 0.5-2.0% depending on the type and extent of the change. Consider offering the Worksheet: Managing Blood Sugars. However, consider this case. e.g. Carl has had diabetes 13 years; his A1c is 11.3%. He wants to work on decreasing his supper pasta from 3 cups to 2 cups. Although this can result in reduced blood glucose levels and weight, the reduction is not likely adequate to bring A1c into target. Still, the behavior should be supported, in addition to the encouragement to pursue further medication adjustment/addition.
- If a trend of hypoglycemia exists secondary to physical activity, it is usually preferable (if the client is agreeable) to decrease diabetes medications rather than increase carbohydrate intake.
- Current medication dose change:
- In the presence of recurrent or severe hypoglycemia, the dose(s) of secretagogues and/or insulin should be reduced. Classes of diabetes medications other than these are not responsible for hypoglycemia.
- Will adusting current medication likely bring them to target or is another agent also needed? E.g. if A1c 10%, client on max metformin with near maximum gliclazide, consider an increase to the latter with a simultaneous request for another agent to be added. Maximum daily doses are outlined in our Complete Diabetes Medications Table.
- Will adusting current medication address the blood glucose pattern
- Are there factors that would suggest a more aggressive dose adjustment (prednisone, minimal effects of last adjustment, obesity)?
- Are there factors that would suggest a more conservative dose adjustment? (frail, low eGFR, inability to self-treat hypoglycemia, lean patient, anticipated rapid weight loss with bariatric surgery, planned significant dietary changes, planned increased exercise, history of severe hypoglycemia, fear of hypoglycemia, etc)?
- What do you anticipate will happen to the glucose pattern after the medication adjustment? Are there safety concerns to address now or when readings drop to a certain level? Eg. Readings are in target except high at bed. An increase to supper repaglinide may require a reduction in overnight basal insulin.
3. Choosing next line agents
- The use of two medications from the same class is generally not indicated E.g. two secretagogues or 2 incretin-based medications (DPP-4 and GLP-1 or Dual GLP-1/GIP Receptor Agonists).
- Educators usually limit suggestions for medication combinations to those indicated in product monographs (per College standards), unless their clinic documents indicate otherwise. The decision to consider an “off-label” (not indicated) combination is the responsibility of the most responsible prescriber (MD, NP, Pharmacist).
- It is a safe practice with respect to College standards to request a separate order to adjust medications when they are used in combinations not indicated in product monographs.
- To learn Health Canada indications and doses, visit the Drug Product Database or our Complete Diabetes Medications Table.
Option A: Use Diabetes Canada's Interactive Decision Tool for Medications - click here.
Use the Interactive Tool and make decisions on the most relevant features for your client.Considerations may include features not listed in The Tool like actual cost/coverage, patient preference, adherence (e.g. once daily vs once weekly dosing) and pregnancy planning,
Option B: Review Diabetes Canada's Visual Resources for Medications
 |
 |
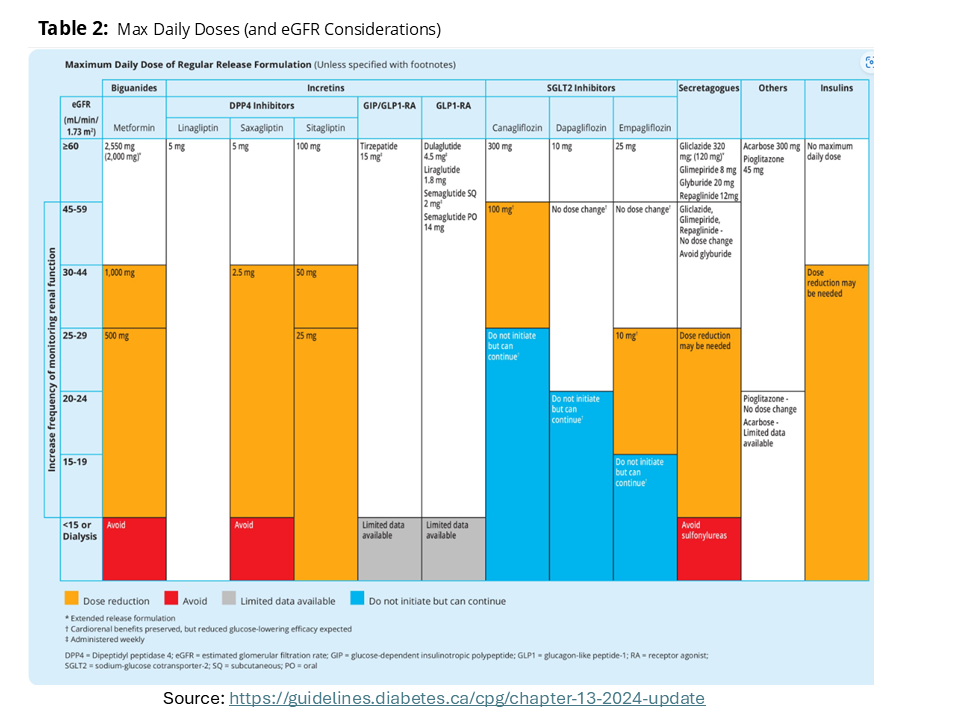 |
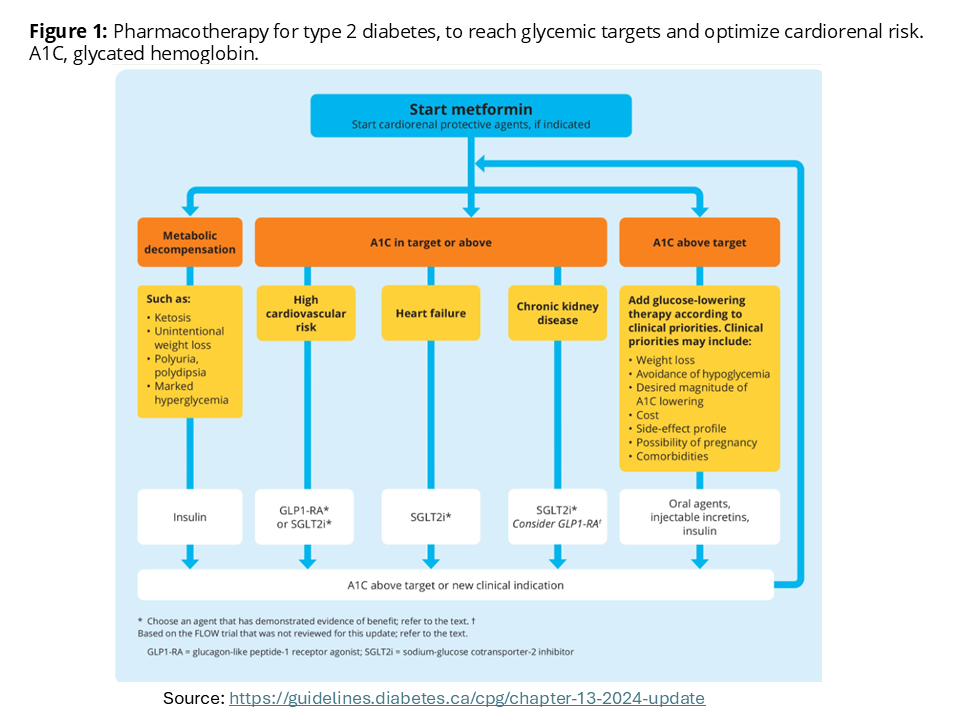
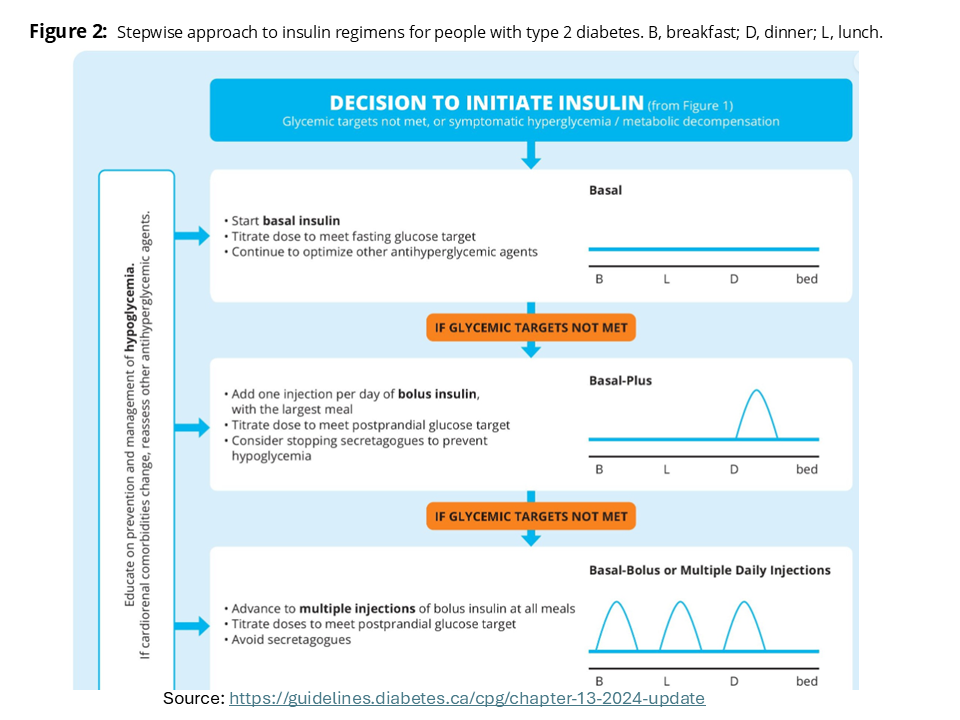
| Figure 1: Pharmacotherapy for type 2 diabetes. Click image for bigger view. | Figure 2: Stepwise approach to insulin in type 2. Click image for bigger view. | Table 1: Daily maximum doses (& eGFR (renal) considerations). Click image for bigger view. |
| Source: Diabetes Canada Clinical Practice Guidelines, Pharmacologic Glycemic Management of Type 2 Diabetes in Adults: 2024 Update | ||
4. Drug Interactions
Patients should review potential drug interactions or side effects with pharmacists when starting any medication. Educators can review interactions in product monographs via Canada's Drug Product Database. A few interactions that impact glycemia are listed below.
Hypoglycemia risk increases with:
- Beta blockers – may decrease symptoms of lows
- Salicylates/NSAIDs – if 4-6 g/day or greater
- Antibiotics: Fluoroquinolones (e.g. ciprofloxacin) can stimulate beta cells to secrete insulin. Hypoglycemia has been reported in patients without diabetes and in patients with diabetes on any antihyperglycemic agent, especially those on insulin or secretagogues.
Hyperglycemia risk increases with:
- Glucocorticoids- including those injected for joints
- Thiazide diuretics – at doses > 25 mg/day