An insulin sensitivity factor (ISF) or correction factor describes how much one unit of rapid or regular insulin will lower blood glucose. For example:
- ISF of 1 means: 1 unit of bolus insulin lowers glucose by 1 mmol/L
- ISF of 2 means: 1 unit of bolus insulin lowers glucose by 2 mmol/L
- ISF of 3 means: 1 unit of bolus insulin lowers glucose by 3 mmol/L
An ISF is used to correct "high" glucose readings. It is individualized and based on total daily dose of insulin (TDD), as well as trial and error.
Quick Reference Formula for Creating an ISF (rapid insulin):
ISF = 100 / TDD
-
Creating an Insulin Sensitivity Factor
Note: TDD = Total Daily Dose of insulin
-
100/TDD = ISF if using rapid insulin (the number of mmol that 1 unit drops glucose in 3-4 hours approx)
-
83/TDD= ISF is using regular/Toronto insulin (the number of mmol/L that 1 unit drops glucose in 3-5 hours approx)
-
EXAMPLE ONE: Teddy, TDD 33, takes rapid insulin
100/33= ISF of 3
1 unit rapid insulin is expected to lower Teddy’s blood sugar by about 3 mmol/L.
-
EXAMPLE TWO: Bear, TDD 80, takes regular insulin
83/80= ISF of 1
1 unit of regular is expected to lower Bear’s sugar by 1 mmol/L. This is aggressive; a safer start may be an ISF of 2.
- For creating Correction Scales, see below.
-
-
Using an Insulin Sensitivity Factor (ISF)
-
Current glucose– target glucose / ISF = units to give to correct the high reading
-
Example: 13 mmol/L – 7 mmol/L target / ISF of 2 = 3 units to correct high blood sugar
-
This correction insulin would be given in addition to the meal bolus (insulin to cover the food).
-
-
Assessing and Changing an ISF
- If ISF results in hypoglycemia, increase it:
ISF 4 becomes ISF 5
ISF 3 becomes ISF 4
ISF 2 becomes ISF 3
ISF 1 becomes ISF 2
If ISF results in above-target readings, decrease it:
ISF 5 becomes ISF 4
ISF 4 becomes ISF 3
ISF 3 becomes ISF 2
ISF 2 becomes ISF 1 -
Assess correction insulin against the ISF formula:
E.g. Sandy has high readings using an ISF of 3. The formula suggests an ISF of 1. In this situation consider a new ISF of 2 to start, as it is safer. If needed, the ISF can change to 1 in the future. -
Assess correction insulin used alone without meal bolus:
If the client took correction insulin but had no meal (no food bulus), assess if it worked. E.g. 12 mmol at breakfast, gave correction but no meal eaten and no food bolus, by lunch was 6.5 mmol/L. This correction worked. Clients are often hesitant to report times they've corrected but missed the meal. Be sure to let them know this could be useful information if they had any to share. -
Assess correction insulin when meal bolus insulin given:
1. First assess if the meal insulin works when in target and no correction insulin is needed.
2. If the meal insulin works when in target, next look for pre-meal readings that are above target. If subsequent blood glucose readings are:
-- In target after giving meal bolus AND correction insulin, the ISF is likely appropriate.
-- High after giving meal bolus AND correction insulin, consider decreasing ISF number by 0.5 or 1.0. E.g. Breakfast 12.0 mmol/L, gave meal and correction insulin, lunch 9.5 mmol/L. Change ISF from 3.0 to 2.0 as an option.
--Low after giving meal bolus AND correction insulin, consider increasing ISF number by 0.5 or 1.0. E.g. Breakfast 12.0 mmol/L, gave meal and correction insulin, lunch 3.3 mmol/L. Change ISF from 2.0 to 3.0 as an option. - Assess Correction Scales - see below
- If ISF results in hypoglycemia, increase it:
-
Correction Scales
Creating Correction Scales
-
If using the ISF is difficult for a patient, consider creating a correction scale. E.g. if an ISF is 2, the left-hand column range for blood glucose readings will increase by approximately 2 mmol/L. If ISF is 3, it will increase by approximately 3 mmol/L.
Sample correction scale: The same correction is given regardless of meal. ISF=2 (meal bolus insulin is not included in this particular chart.) If using mobile, turn phone sideways.
If blood sugar is: Give this many extra units of rapid insulin along with your usual meal insulin. 7.1-9 mmol/L 1 unit 9.1 – 11.0 mmol/L 2 units 11.1 – 13.0 mmol/L 3 units 13.1 – 15 mmol/L 4 units - Correction doses may be the same for each meal, as per the scale above, or they may differ per meal based on trial and error. See the scale below for an example of the latter.
Sample correction scale: Different correction is advised per meal. ISF=2 (meal bolus insulin not included in this sample chart). If using mobile, turn phone sideways.
If blood sugar is: Breakfast Lunch Supper 7.1-9 mmol/L 1 unit 2 units 2 units 9.1 – 11.0 mmol/L 2 units 2 units 2 units 11.1 – 13.0 mmol/L 3 units 3 units 4 units 13.1 – 15 mmol/L 4 units 4 units 4 units
Adjusting Correction Scales
- Method 1 Correction Scale Adjustment:
Analyze the correction scale in sections. First, verify that the meal dose works (e.g. when 4-7 mmol/L before meals and no correction is given.) Then check to see if the dose recommended when e.g. 7.1- 9.0 mmol/L at breakfast works; the same for 9.1-11.1 mmol/L works etc. This can be time consuming as it requires repeatedly skimming large amounts of data numerous times to identify readings within certain ranges. The second method below is often shorter and easier. - Method 2 Meal Bolus + Correction Scale Adjustment:
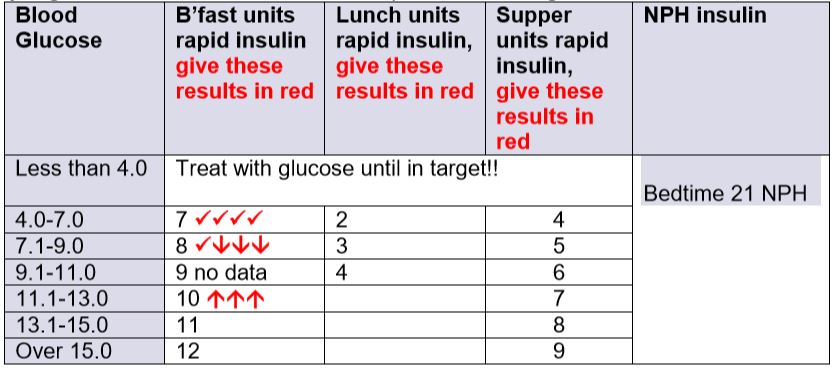
Indicate with checkmarks or arrows how each section of the scale is performing. In the example below, the units in each cell include the meal bolus + correction added together.
For example, if before breakast is 11.2 mmol/L, but before lunch is still 11.2 (above target, and no morning snack), that part of the breakfast scale is coded with an arrow up, as it gave a reading above target. It would be coded with an arrow down if resulted in hypoglycemia or coded with a checkmark if resulted in a reading that was in target. Repeat for all readings for each of the meal times (don't use readings like "ate extra this meal" or "shopped ++").
This is a relatively quick way to analyze the cells in an insulin scale or algorithm. It can be done alone by the educator or together with the patient's help. (Have the patient read out the breakfast glucose result, ask them to pause, then read out the same day's lunch reading, and pause. It's a novel way to get patient participation.)
When finished, analyze the pattern of arrows and checkmarks to determine which parts of the scale need adjusting. In the partically completed example above, the 4-7 mmol/L part of the scale at breakfast gives results that are in target. The 7.1-9.0 mmol/L section at breakfast (8 units) gives mostly hypoglycemic results, so needs decreasing (e.g.to 7 units); whereas the 11.1-13.0 mmol/L part of the breakfast scale (10 units) gives results that are above target so that dose needs increasing (e.g.to 11 units or more).
5. Supplemental Notes
-
The ISF is usually dependent on the individual’s sensitivity to insulin. A person more sensitive to insulin is likely to have a larger number for ISF (eg. 3, 4 or occasionally 5). A person with insulin resistance is likely to have a lower number for ISF (eg. 1 or less than 1).
-
An ISF of 1 (1 unit to drop 1 mmol/L) is usually not safe to start, although a very insulin resistant client may eventually require that. An ISF of 2 (1 unit to drop blood glucose 2 mmol/L) is common and would be safer to try initially, than an ISF of 1. In lean people with established type 1 diabetes, an ISF of 3-4 is not unusual. An ISF of 5 may be needed in early type 1 diabetes, although high readings may often “self-correct” in those who are honeymooning and still making endogenous insulin.
-
Corrections after meals are often not suggested, to avoid “stacking” insulin. However, if required, advise to correct to a post meal target eg. of 10 mmol/L. E.g. Current glucose– target glucose of 10 / ISF = units to give to correct the high reading after a meal.
-
As with any insulin formula, expect that results can vary at times.
-
ISF values, particularly in insulin pump therapy, may also be developed using fractions e.g. an ISF of 1.5 (1 unit drops glucose 1.5 mmol/L).